Voice Restoration Through Vertical Partial Laryngectomy in Laryngeal Amyloidosis Patient: A Case Report
Article information
Abstract
Amyloidosis is a idiopathic clinical syndrome caused by deposition of non-soluble protein fibers in the extracellular matrix of organs and tissues. It causes chronic inflammation and destruction of the architecture and functionality of the involved tissue. Amyloidosis occurring in the upper airway tract is rare, accounting for 0.2% to 1.2% of benign tumors of the larynx. In general, the purpose of treatment is reduce the risk of dysphagia and dyspnea. Endoscopic surgery is the mainstream of the treatment because laryngeal preserving is the most important goal of treatment. However, the disadvantage of this treatment is that it can lose voice and may require multiple reoperation. In this article, we report a case in which vertical partial laryngectomy (VPL) in a patient with laryngeal amyloidosis, because the patient want her voice restoration. It was observed that voice restoration and airway patency were maintained for two years without additional surgical treatment after the surgery. Although additional studies are needed, VPL can be a good option for patients who want to preserve their voice.
INTRODUCTION
Amyloidosis is a group of idiopathic clinical syndromes caused by deposition of nonsoluble protein fibers in the extracellular matrix of organs and tissues [1-3]. It causes chronic inflammation and destruction of the architecture and functionality of the involved tissue [4]. Today, amyloidosis is classified into two groups depending on its characteristics as systemic amyloidosis and localized amyloidosis [5]. In addition, the type of amyloidosis can be divided into subgroups, such as immunoglobulin kappa and lambda light chain, serum amyloid A and β-2-microglobulin amyloidosis, and so on [6,7]. Localized amyloidosis can be identified in any part of our body, including the nasopharynx, oral cavity, oropharynx, larynx, and salivary gland [8,9]. Amyloidosis occurring in the upper airway tract is rare, accounting for 0.2% to 1.2% of benign tumors of the larynx [10,11]. Symptoms of this disease range from hoarseness, dysphagia, and cough to dyspnea and wheezing depending on its aggravation [8]. Treatment method of laryngeal amyloidosis has not been established yet. In general, the purpose of treatment is to preserve voice and reduce the risk of dysphagia and dyspnea [3,12]. Endoscopic surgery using cold steel, coblation, or CO2 laser is the mainstream of the treatment [8]. Larynx preserving is the priority of treatment. Thus, surgery should be focusing on debulking and reducing symptoms of laryngeal amyloidosis rather than complete excision of the affected lesion [13]. For functional preservation, it is important to preserve laryngeal structures such as anterior commissure and thyroarytenoid muscle [7]. The external approach is rarely used except for severe cases that need complete surgical excision [9,13]. Recently, low dose radiotherapy has been studied for its effectiveness in amyloidosis. Its effectiveness is controversial, requiring long-term evaluation [14]. We reviewed one case of localized laryngeal amyloidosis treated with vertical partial laryngectomy (VPL).
CASE REPORT
An 83-year-old female with dyspnea was referred to a tertiary hospital for further evaluation via a local clinic. She did not have any comorbidities. Laryngoscopy revealed yellowish colored irregular surfaced mass at left vocal cord (Fig. 1A). Clinical findings suspected amyloidosis. Laryngeal microsurgery was scheduled. Histopathology confirmed amyloidosis as a result of positive congo red staining. However, she was lost to follow-up for six years. She revisited our hospital due to progressive worsening dyspnea and loss of her voice. Physical examination revealed stridor, sternal retraction. Laryngoscopic exam showed severely narrowed airway compared to past laryngoscopic image. The vocal cords on both sides were severely adhered, with no glottic gap (Fig. 1B). We performed emergent tracheostomy. Her symptoms improved. However, careful surveillance was required to determine whether the disease had progressed or not. She complained of loss of her voice at five months after tracheostomy. Further laryngoscopic exam and computed tomography (CT) showed total obstruction of the larynx (Figs. 1C and 2). In general, endoscopic surgery using microdebrider or CO2 laser is chosen for airway stenosis caused by amyloidosis. However, as her airway showed totally obstructed state, we decided to perform open VPL. After vertical skin incision and subplatysmal flap elevation, vertical incision was done at the midline of thyroid cartilage. The mass was noted mainly on left ventricle and true vocal cord, invading the anterior commissure. Synechiae formation and total glottic stenosis were identified. Thus, we decide to remove left vocal cord and reconstruct it using bipedicled thyrohyoid muscle flap. A VPL was performed on the left vocal cord to preserve vocal cord function (Fig. 3). After surgery, her voice was recovered and airway patency was improved, with tracheostoma remained (Fig. 2). Our patient did not show symptoms of systemic amyloidosis such as bone pain, night sweats, lymph nodes enlargement, or splenomegaly. Her serum and urine electrophoresis results were normal. Three months after surgery, laryngoscopy was performed to evaluate the amyloidosis lesions. Compared to the preoperative condition, the right vocal cord exhibited normal movement, while the left vocal cord showed the typical degree of movement observed after VPL (Fig. 1D). Over the two years following the surgery, there has been no recurrence of laryngeal amyloidosis, and her voice has been maintained. Complications such as dysphagia and aspiration were not present. However, due to relatively narrow glottic gap, decannulation has not been performed, and she continues to use an tracheostomy retainer.
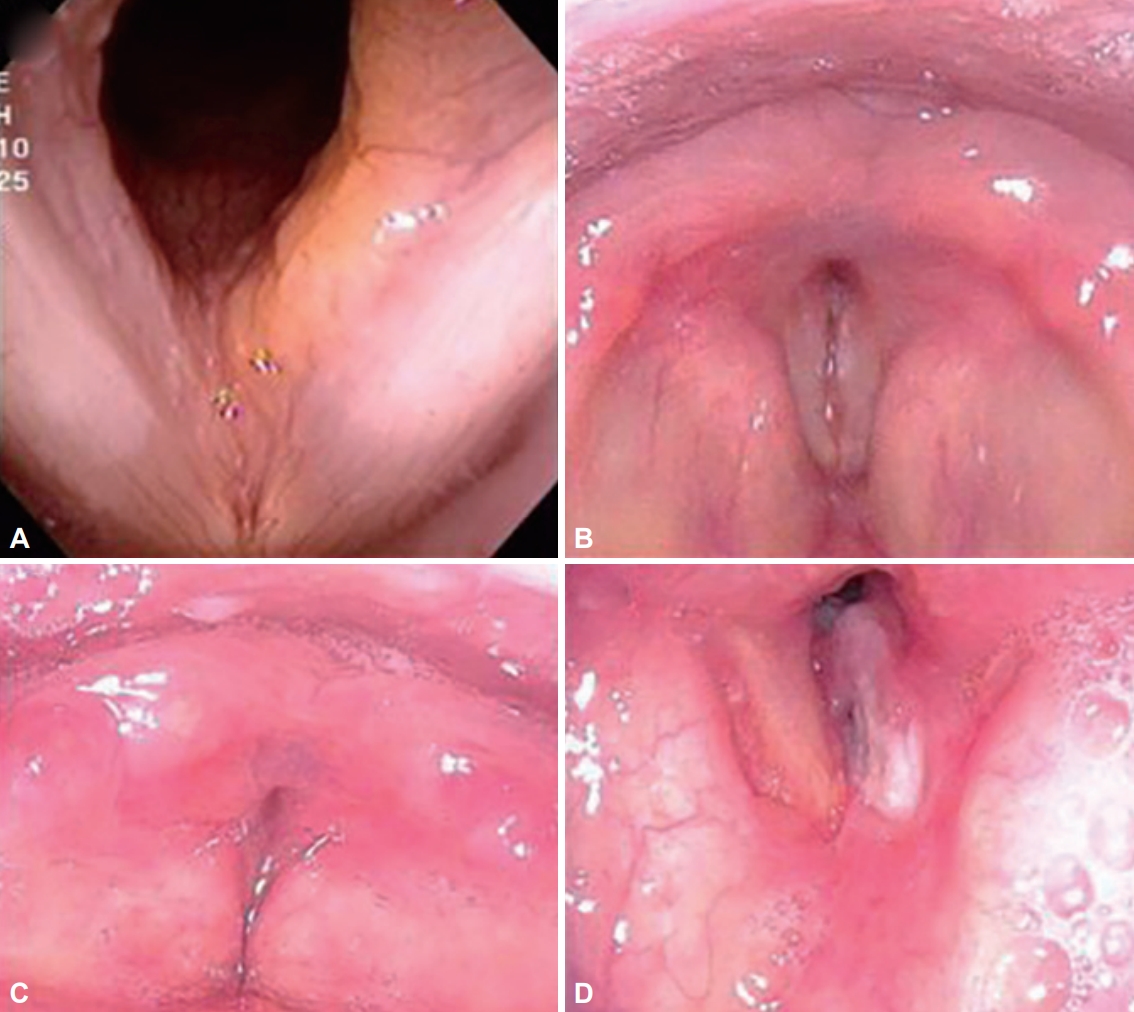
Laryngoscopic image of the patient. A: Laryngoscopic image when the patient first visited the hospital. B: Laryngoscopic images before tracheostomy. C: VPL. D: Laryngoscopic image after VPL. VPL, vertical partial laryngectomy.
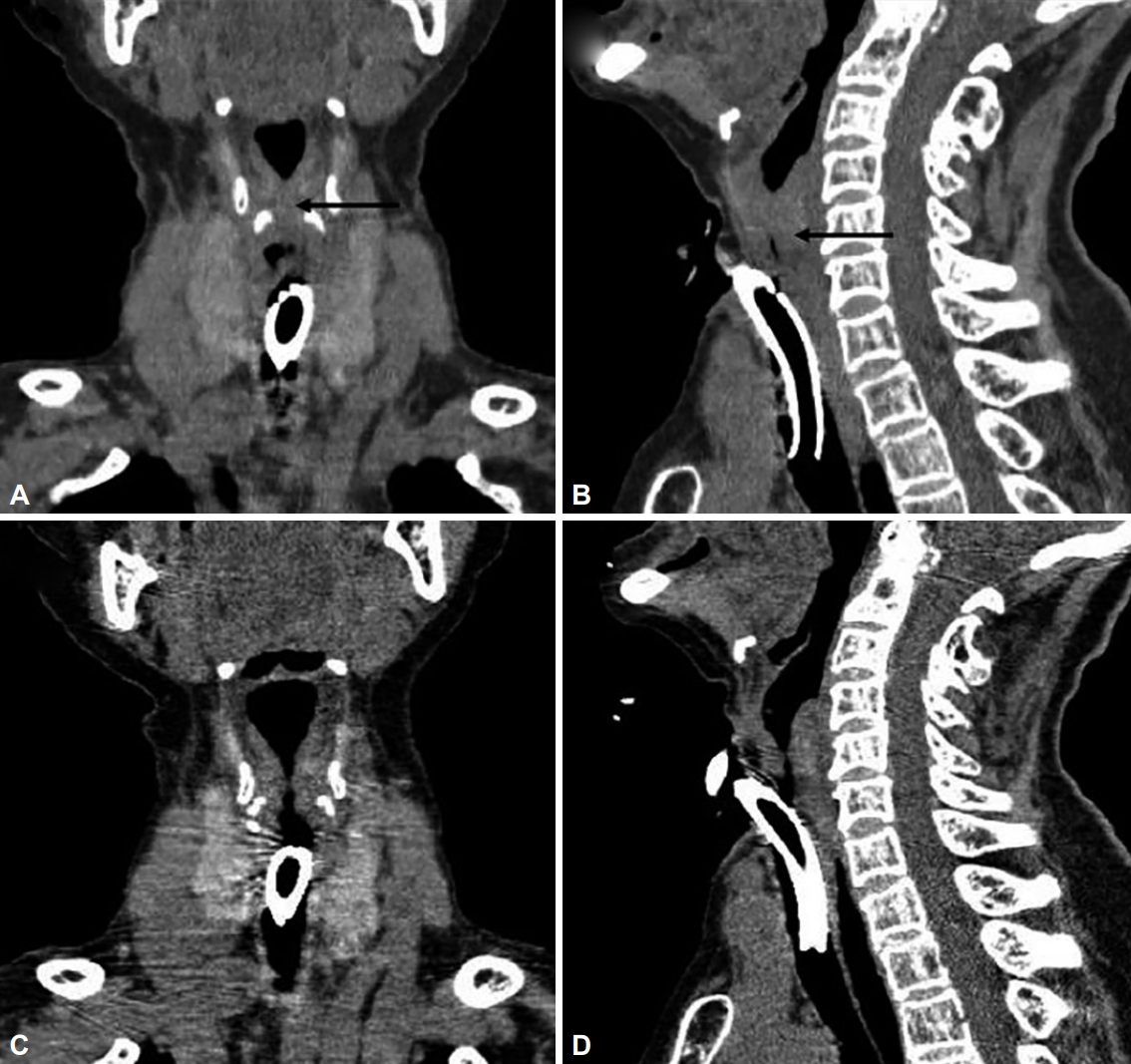
CT image of the patient. Coronal (A) and sagittal (B) CT images before VPL showing total obstruction of larynx. The black arrow points to the amyloid lesions. Coronal (C) and sagittal (D) CT images after VPL showing glottic gap. CT, computed tomography; VPL, vertical partial laryngectomy.
DISCUSSION
Amyloidosis was first described by Virchow as accumulations of fibrillary proteinaceous substances in various kinds of tissues [8]. These protein fibers’ beta-pleated sheet ultrastructure shows apple green color under a polarization microscopy when stained with Congo red [8,11]. Therefore, the gold standard for the diagnosis of amyloidosis can be made through histological examination obtained through biopsy [1].
Long-term follow-up studies of amyloidosis in the upper airway show that no patient develops systemic amyloidosis, B-cell lymphoma, or multiple myeloma [14,15]. However, systemic amyloidosis has a worse prognosis than local amyloidosis. Thus, systemic examination is essential. Main symptoms of this disease are dysphonia, throat discomfort, dyspnea, and asymptomatic. These symptoms depend on the location of the lesion. The most frequently involved laryngeal sites are laryngeal ventricles, false vocal cords, genuine vocal cords, aryepiglottic folds, and vocal cords [12]. Since laryngeal amyloidosis is mostly a submucosal disease, imaging techniques such as CT and magnetic resonance imaging can help determine the extent of lesion involvement [9]. These radiological scans can help identify lesions of submucosa from normal soft tissue in the neck, which are not easily identified by physical examination or laryngoscopy [6]. Because of its rarity, just a small case series of case report are mainstream of document. Until recently, only a few treatments have been reported, from local excision to total laryngectomy [13,16]. The purpose of treating laryngeal amyloidosis is to increase time phonation and breathing as much as possible. There are conflicting opinions on the choice of treatment. In previous studies, researchers have stated that radical excision of lesions through extensive resection is more effective, while others have indicated that local resection alone can achieve sufficient effect [13,16]. Because of the effectiveness of local excision, endoscopic removal of lesions using microdebriders or CO2 lasers is main stream of the treatment. However, the effect of local excision is temporary. It often recurs. Thus, repeated surgery is often required. Mesolla et al. [1] have reported five laryngeal amyloidosis patients through endoscopic surgery. All patients were followed up monthly for six months. Four patients showed immediate improvement in symptom after surgery. However, one patient needed further treatment. Treatment of amyloidosis should be selected base on the extent of the lesion. Endoscopic surgery allows rapid improvements and short hospitalization time.
We needed to use an external approach for this patient because her larynx showed near total obstruction. In this patient, the lesion invaded both ventricles through the true vocal cord. Thus, preserving the laryngeal function was challenging. We performed VPL as a way to maintain airway patency and preserving voice for a long period of time. Laryngofissure approach, supraglottic laryngectomy, and even total laryngectomy have been performed in some severe cases [5,16]. It was observed that voice restoration was maintained for two years without additional surgical treatment after VPL. However, there are several limitations. Long-term follow-up is required to compare effects of VPL and other surgical resections. Also, it is necessary to compare whether functional aspects of patients through more cases. Due to the rarity of this disease, further studies can be difficult.
Acknowledgements
None
Notes
Ethics Statement
IRB was waived by the institution (2023-10-051).
Funding Statement
This paper was supported by Fund of Biomedical Research Institute of Jeonbuk National University Hospital.
Conflicts of Interest
The authors have no financial conflicts of interest.
Authors’ Contribution
Supervision: Yong Tae Hong. Writing—original draft: Hyunjun Lee. Writing—review & editing: Yong Tae Hong, Hyunjun Lee. Approval of final manuscript: Yong Tae Hong.

